The Ins and Outs of Intrauterine Devices
Your guide to choosing the right IUD for your body

Key Takeaways
- There are 5 different IUDs available: 4 are hormonal, and 1 is non-hormonal.
- The IUDs differ in size and dosage.
- IUDs are more than 99% effective at preventing pregnancy.
- They can also be used to prevent heavy, painful periods or abnormal bleeding.
IUDs (or intrauterine devices) are one of the most convenient and effective forms of contraception and cycle regulation available. But even among IUDs, there are so many different types to choose from! Knowing your options can help narrow down what is most important to you and help you find the right fit.
What is an IUD?
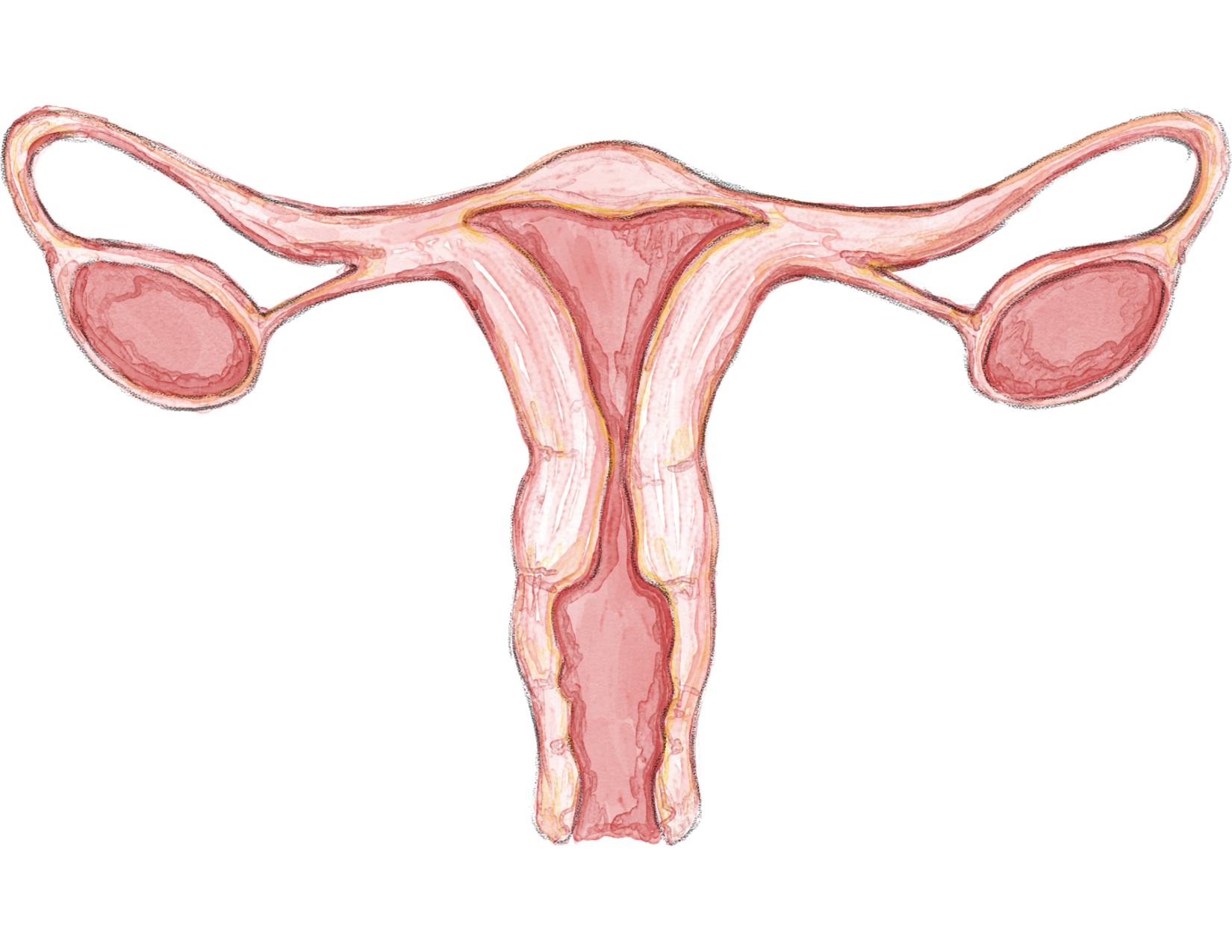
An IUD is a T-shaped device that is placed into the uterus by a healthcare provider. It is a type of long-acting reversible contraceptive (LARC). Let’s break this term down:
- Long-acting: IUDs last for several years, ranging from 3 years to 12 years depending on which IUD is placed.
- Reversible: IUDs can be taken out at any time. Once your IUD is removed, your cycles should go back to how they were before your IUD within a few weeks or even sooner. Return to fertility is immediate for most people; many are able to become pregnant very quickly after removing IUDs.
- Contraceptive: IUDs can be used for pregnancy prevention. And IUDs are particularly good at their job – around 99% effective.
It’s worth noting that IUDs do not protect against sexually transmitted infections (STIs, sometimes better known as STDs). If you wish to lower your risk of STIs, use barrier methods like condoms or dental dams, and get tested regularly. IUDs are mostly used for preventing pregnancy or for treating painful, heavy periods.
For transgender and nonbinary folks, having a period can trigger gender dysphoria. Since some IUDs can be used to help stop or lessen menstrual bleeding, IUDs can be part of gender-affirming care.
Certain IUDs can also be used as emergency contraception. Oral emergency contraception, such as Plan B and Ella, are not as effective for certain bodies. IUDs, on the other hand, can be used regardless of weight or BMI, and have an extremely high effectiveness (near 100%).
What are the different types of IUD?
There are two main categories of IUD: hormonal, and non-hormonal.
The hormonal IUDs contain the hormone levonorgestrel, a form of progestin. There are four different types of hormonal IUDs: Skyla, Kyleena, Liletta, and Mirena.
For your information
What is progestin? Progestin is the synthetic version of the hormone progesterone. Progesterone is made by your body and is one of the hormones that supports menstruation and early pregnancy.
One thing to note about hormonal IUDs is that they often work for people who have negative side effects from pills, patches, rings, or other hormonal methods. The hormones in IUDs stay fairly localized (aka in your uterus). Because there is no estrogen, headaches are far less common. They also work well for people who have migraines with aura that are unable to use estrogen-based methods. Of course, everyone’s bodies are unique. There may be some trial and error no matter what method you choose.
The non-hormonal IUD, also known by its brand name Paragard, is made with copper.
These five options differ from one another in size, duration of use, and side effects. Each has a unique set of factors to consider when deciding the right option for you. Unfortunately, it is hard to predict how someone’s body may react to a type of birth control. However, this article will give you a starting point so you can talk to your provider about what you think might work for your unique body.

For your information
Only 8-12% of people report having any headaches from IUDs.
Paragard
How does Paragard work?
Paragard is the only non-hormonal IUD on the market. The Paragard IUD is wrapped with copper, which is toxic to sperm and egg cells. It creates an environment in the uterus that is inhospitable for a pregnancy.
How long does Paragard last?
Paragard is FDA-approved for 10 years of use, but evidence shows that Paragard is safe and effective for even longer.
Can Paragard be used as emergency contraception?
Yes! Paragard can be used as emergency contraception if placed within 5 days (120 hours) of unprotected intercourse. It is more than 99% effective.
How do I know if Paragard is right for me?
Paragard is a good option for anyone who prefers to limit exogenous (outside) hormone exposure for any reason, including:
- People with health conditions that prevent them from using hormonal birth control
- People who feel nervous about how altering their hormones will make them feel
- People who have had bad reactions to other hormonal birth control methods
- Anyone looking for an effective, non-hormonal birth control option
For people with heavy and painful periods, Paragard might not be the best choice. Paragard causes an inflammatory response in the uterus. This may result in more intense cramping and heavier period flow. For some people these changes last only the first 3-6 months. For others, they last longer.
Anyone who has a history of severe iron-deficiency anemia should take caution before having Paragard placed. Paragard may worsen anemia due to a heavier period flow.
Mirena / Liletta
How do Mirena and Liletta work?
Mirena and Liletta are two different brands of very similar IUDs. They are both hormonal IUDs and contain 52 mg of the hormone levonorgestrel. A small dose of levonorgestrel is released from the IUD every day in order to maintain a steady state of the hormone in the body.
Levonorgestrel IUDs work in a few different ways. The hormone thickens cervical mucus which makes it very difficult for sperm to travel to an egg. It also helps keep the lining of the uterus super thin, which prevents eggs from attaching to the uterine wall.
How long do Mirena and Liletta last?
The Mirena and Liletta are each approved for up to 8 years for pregnancy prevention.
Can Mirena and Liletta be used as emergency contraception?
Yes! Both Mirena and Liletta can be used as emergency contraception if placed within 5 days (120 hours) of unprotected intercourse. Both are more than 99% effective.
How do I know if Mirena or Liletta is right for me?
One of the most common side effects of levonorgestrel IUDs is irregular bleeding. However, for many people using Liletta or Mirena, periods become much lighter. In fact, many people with these IUDs don’t experience monthly bleeding at all. For this reason, Liletta or Mirena can be a great option for people with painful or heavy periods, breakthrough bleeding, or iron-deficiency anemia. Mirena is actually FDA-approved to treat abnormal uterine bleeding for up to 5 years.
Mirena and Liletta are also great options for transgender or non-binary people who wish to stop or lessen their periods. The level of levonorgestrel in these 2 brands is the highest out of the hormonal IUDs and therefore most likely to affect menstrual cycles.
People who prefer to have regular monthly periods may find that their cycles are really different on the Mirena or Liletta IUDs. If skipping periods or experiencing irregular spotting would stress you out, it might be better to choose another method.
For your information
It's totally okay to get your IUD inserted or removed while you're on your period!

Skyla
How does Skyla work?
The Skyla IUD contains levonorgestrel, and functions in the same way as the other hormonal IUDs. The difference is that Skyla is smaller in size, and has a lower dose of levonorgestrel.
How long does Skyla last?
Skyla is approved for 3 years of use.
Can Skyla be used for emergency contraception?
Due to the lower amount of levonorgestrel, Skyla is not used as emergency contraception.
How do I know if Skyla is right for me?
Skyla was specifically tested in people who have not been pregnant before. It is slightly smaller in overall size to fit into a smaller uterus. This may make it a good choice for teenagers.
Skyla would also be the right fit for someone looking for a hormonal IUD with the lowest possible hormone dose.
For someone looking for a birth control method that completely stops periods, Skyla might not be the best option. At the end of the first year of use, only 6% of people using Skyla stopped getting periods (as opposed to 19-20% of Liletta and Mirena users).
Kyleena
How does Kyleena work?
The Kyleena IUD contains levonorgestrel, and functions the same way as the other hormonal IUDs. It is the same size as Skyla. What makes Kyleena unique is its hormone dose. The levonorgestrel dose of Kyleena falls between that of Mirena/Liletta and Skyla at 19.5mg.
How long does Kyleena last?
Kyleena is approved for 5 years of use.
Can Kyleena be used for emergency contraception?
Due to the lower amount of levonorgestrel, Kyleena is not used for emergency contraception.
How do I know if Kyleena is right for me?
Kyleena is great for someone looking for a longer-lasting, smaller IUD. Some people with Kyleena have lighter bleeding overall, and many do not get periods with Kyleena in place. This IUD may be worth trying, regardless of pregnancy history, for people who are looking for a slightly smaller and lower dose option with similar benefits to the Mirena or Liletta.

How can I prepare for my IUD insertion?
We’ll be honest: for most people, the IUD insertion process is pretty uncomfortable. Most people describe feeling sensations similar to intense menstrual cramping.
If you are worried about the pain, here are a few ways you can advocate for yourself:
- Talk to your provider about taking ibuprofen or acetaminophen about an hour before your appointment.
- Talk to your provider about other pain relief options for your procedure, including numbing medications for your cervix. Every clinic has different options available. Your provider can help you figure out which, if any, is best for you.
- Ask for a heating pad. You can place a warm compress or hot pack over your pelvis before and after the insertion to help with cramping.
- Squeeze a stress ball during the insertion process. IUD insertions can sometimes cause a vasovagal response. This is a nervous system reaction that may cause you to feel nauseous, sweaty, shaky, and sometimes even faint! It can feel really intense. “Isometric contraction” of the muscles of your arm can intervene to help stop a vasovagal response.
- Make sure you are well-hydrated and have eaten the day of your procedure. You are more likely to have a vasovagal response if you are dehydrated and/or hungry!
- If you are at risk of becoming pregnant, make sure you use condoms or another type of birth control for at least 2 weeks before you have your IUD inserted. If you do have sex that could result in pregnancy, talk to your provider about having your IUD inserted as soon as possible. Some IUDs can be used as emergency contraception for up to 5 days after unprotected sex, but not all.
If you’re feeling stressed about the whole process (and not just the pain), here are a few suggestions for making yourself more comfortable:
- Come with a trusted friend or family member. This person can hold your hand, distract you or comfort you during the procedure, and help you get home afterwards.
- If you can't bring a support person, consider other things that might make you feel calmer, like your favorite music or cute videos of cats! If you are feeling very anxious about the insertion, talk with your provider beforehand about options to decrease your anxiety.
- Another option is to ask for a support person from the clinic’s team. Most clinics are happy to provide a staff member to hold your hand or chat with you during the procedure.







